Private prescriptions in UK Private Healthcare
Discover how prescriptions are done in the UK.
Private prescriptions in UK private healthcare – How they work, how they are evolving
By Dr. Sean Brink, GP
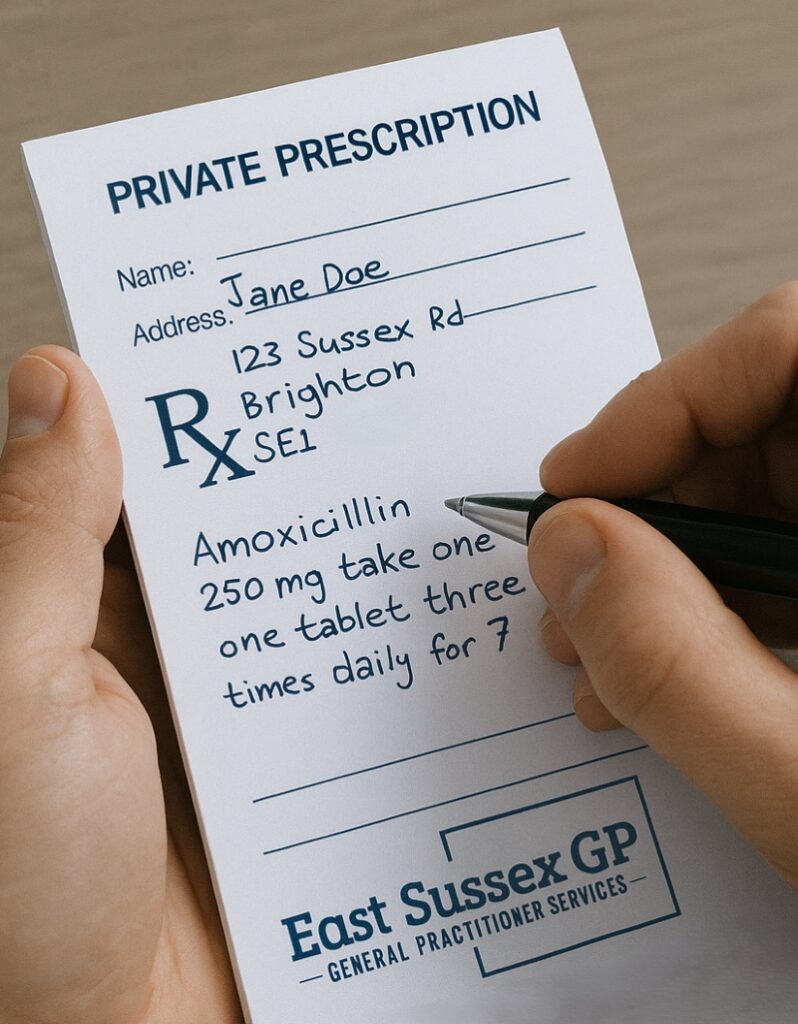
In the UK, patients who access private healthcare (for example through a private GP or telemedicine service) may receive a private prescription rather than an NHS prescription.
Unlike prescriptions issued under the NHS, private prescriptions (sometimes called “self-funded” or “pay-as-you-go” prescriptions) are entirely paid for by the patient.
“This service saved me so much time. I didn’t need to travel back to the clinic or wait for paperwork. The digital prescription worked perfectly at my nearest pharmacy.”
Patient
What makes a prescription “private”?
Here are some key features and implications of private prescriptions:
It is not issued on the NHS FP10 stationery (for NHS prescriptions) and is not funded by the NHS.
The prescriber (often a private GP, private consultant) issues the prescription on the basis of a private consultation or arrangement. The patient pays for the consultation / service, and then pays for the medication at the pharmacy.
A private GP cannot convert a private prescription into an NHS prescription simply because a patient prefers it; and NHS-registered GPs cannot ordinarily issue private prescriptions for their regular NHS list patients under the GMS contract rules in respect of standard NHS medicines.
Why do patients use private prescriptions / private GP services?
Private GP services often offer faster access, longer consultation times, more flexibility (evening/weekend/remote) and a more “premium” patient experience.
Private prescriptions offer access to medications or services not routinely funded on the NHS, or accessed via private providers.
The arrival of specialised digital prescribing platforms means the process is more streamlined, efficient and patient-friendly.
How the issuing of a private prescription works
Within a private consultation, a prescriber will assess the patient (face-to-face or remotely) and decide that a medication is clinically appropriate. They then issue a private prescription. The patient takes (or is sent) the prescription to a pharmacy and pays for the cost of the medication plus usual dispensing fees.
For a private GP practice instead of hand-writing a script, scanning it, or posting it, the clinician can issue a prescription ID token or digital script by email or phone SMS within minutes. Platforms like SignatureRx and CloudRx are designed with this in mind.
https://signaturerx.co.uk/patient-guide/
From the patient’s perspective:
A remote or face-to-face private appointment may conclude with a prescription token emailed or phone SMS text to them.
They can present the prescription ID token at any UK pharmacy of their choice (depending on contract) or have the medication delivered to their home.
They will pay the full cost of the medication (private prescription cost) plus any dispensing fee; this may be higher or lower than the NHS prescription charge depending on the medicine
For more information also see https://www.cloudrx.co.uk/how-it-works
Limitations, regulatory issues and particular cautions (especially for controlled drugs)
While private prescriptions provide flexibility, there are important regulatory boundaries and safety considerations — especially for controlled drugs (CDs), for long-term monitoring of medicines, and for interface with NHS care.
Controlled drugs: For private prescribing of CDs, additional requirements apply (e.g., use of FP10CD forms ). The guidance from the NHS Business Services Authority and Home Office states that private prescriptions for Schedule 2 and 3 CDs must be written or have special storage and submission arrangements.
So when a private clinic is providing medication that is a CD (e.g., certain opioids, benzodiazepines) the usual paper-based or regulatory compliant form must be used, and the dispensing pharmacy must submit the forms appropriate. Prescribers are regulated by the regional CD accountable officer.
Long-term monitoring: If a medication requires ongoing monitoring (for example blood tests for monitoring organ function, drug levels, or side-effects) then simple issue of a prescription may not suffice. The private prescriber must ensure that monitoring is arranged (either within their own service or via a shared care agreement with the patient’s NHS GP). Some NHS practices have policies explaining they may not agree to take over prescribing of a medication recommended by a private specialist unless they have the relevant letter, monitoring protocols.
Shared care / handover: If a private prescribing arrangement is ongoing, it may make clinical and financial sense to hand over long-term prescribing and monitoring to the patient’s NHS GP by means of a shared care or referral arrangement — provided the NHS GP agrees. Without this, the private clinic may need to continue responsibility for monitoring. It is the prescribers responsibility to ensure patients understand this and important to clarify this at initiation of treatment.
Scope and cost: Private prescriptions are not automatically cheaper than NHS items; indeed the patient pays full cost. Some medications may not be available on the NHS except under specific criteria, so private prescribing may be the only route. But the patient must be aware of cost, availability, and pharmacy dispensing policy. The patient’s NHS GP may decline to take over prescribing of a privately initiated medication if they feel it is not appropriate or they do not have adequate information.
Continuity of care: If the patient remains registered with an NHS GP (as is common), the private prescriber and the NHS GP need to ensure effective communication of prescribing decisions, monitoring plans, and any changes. Private care should not work in isolation without communication with NHS care if the patient has other comorbidities or ongoing NHS care.
Key considerations for private prescribing via your service
Ensure clinicians holds the correct prescribing qualification and is registered to prescribe privately.
-
Confirm your selected digital prescription platform (SignatureRx, CloudRx, etc) meets regulatory requirements for the type of medicine being prescribed (especially CDs).
-
When issuing private prescriptions, make clear to the patient they are paying for the prescription and medication, and that NHS prescription charges do not apply.
-
For medicines requiring ongoing monitoring (e.g., liver/kidney function, drug levels, specialist review), clarify who will do the monitoring (private clinic/internal; or handover to NHS GP) and document this in the care plan.
-
For controlled drugs, limit supply to no more than 30-days (unless clearly justified), ensure safe prescribing and storage, and ensure the pharmacy and prescribing platform manage the regulatory submission of the forms (FP10PCD/FP34PCD) in a timely manner.
-
Provide patient education about the prescription: how to redeem (token or pharmacy), how to pay, what happens if they change pharmacy, what happens if they later need to transfer prescribing back to NHS GP.
-
Maintain clear communication and documentation between your private service and the patient’s NHS GP (if applicable), especially if the medication is long term or high risk. Patients registered with an NHS GP should not be left on “orphan” prescriptions without oversight.
-
Be clear about limitations: a private prescription does not guarantee the NHS GP will agree to continue it; the patient may have to continue paying or revert to NHS-approved alternatives.
Conclusion
The private prescription pathway in the UK is a viable and increasingly streamlined route for patients accessing private healthcare.
With digital platforms like SignatureRx and CloudRx, the patient journey is becoming faster, more convenient and better suited to remote or hybrid models of care.
However, safe, appropriate prescribing, robust monitoring (especially for long-term therapy or controlled substances), and clear interface with NHS care remain essential pillars of good practice.
Dr. Sean Brink is a General Practitioner committed to enhancing patient engagement and promoting digital health solutions for patients.
